In Search of the Hospital District Subsidized “Primary Care Clinic”
by Martha K. Huggins, Ph.D…….
Be Compassionate and Giving; Welcome the Stranger. The sacred texts of major world religions—Buddhism, Christianity, Catholicism, Hinduism, Islam, and Judaism—talk of the inherent goodness of the poor and extol followers to welcome the stranger and assist the needy. Capitalism– in most of the modern world–elevated to that of a religion, considers poor people risky, a nuisance, and fiscally dangerous: Mere ‘things’ requiring “risk management.” Contracts are written and legal opinions delivered, to protect corporate wealth and its very well-paid executives from the imagined exactions that the poor, poorer, and indigent allegedly pose to capital’s bottom line.
Case in point, the Lower Keys Hospital District Board, created by the State in 1967, is the government body responsible for the hospitals in the Lower Keys’ district. The Board paid Attorney Maria Currier, Esq., Partner at Holland & Knight’s Miami office, $25,000 dollars (for some workers an annual salary) to render a legal opinion about the Hospital District’s 1999 contract[i] with the for-profit corporation, Health Management Associates (HMA) to lease and operate the local hospitals.
Attorney Currier’s opinion focused only on the legality of leasing out the not-for-profit Memorial Hospital (5900 College Road) to HMA, a for-profit corporation, thus changing Memorial Hospital into a for-profit medical center – the Lower Keys Medical Center [LKMC]: Opinion: “The [Hospital] District was statutorily authorized to enter into the lease [with the for-profit HMA] and to delegate all of the Hospital Operating Decisions to HMA.” Opinion: “The Hospital District is preclude[d]…from retaining responsibility for Hospital Operations Decisions.” Opinion: “By HMA[’s] assuming the indigent care obligations of the District, without limitation, there is no need for the District to levy ad valorem taxes on the District’s residents over the entire 30 year term of the lease.”[ii]
But has HMA [now CHS, Community Health Systems], in fact, assumed the indigent care obligations of the District? This question is not strictly answerable since CHS is protected from responding to public information requests since the “Sunshine Law” does not apply to private entities like CHS. Florida Statute 155.40 is clear that, in “a sale or lease of a county, district, or municipal hospital,” there is an “enforceable commitment that programs and services and quality health care will… be provided to all residents of the affected community, particularly to the indigent, the uninsured, and the underinsured.”
The contract between the District and the for-profit company specifically demands that the company provide not only the statutory required indigent care at its hospitals, but also a Primary Care Clinic for all residents of the district including those that can’t pay.
“The clinic shall provide a broad range of primary care health services with an expanded operating schedule to all Residents regardless of the Resident’s ability to pay.”
The contract required HMA/CHS to furnish the space for the Clinic and all non-physician personnel; the District is obligated to fund the cost of physician services for the clinic’s indigent patients [up to a maximum of $500,000 per year].
“All administrative and non-physician allied health professional staff will be provided by Lessee. The physician coverage for the Clinic will be provided by participating physicians (at no cost to Lessee) practicing in the Lower Florida Keys Hospital District… Lessee will be obligated to maintain the space for the Clinic for the lease term and may only discontinue providing such space and administrative support prior to expiration of the lease term with approval of the Lessor…”
Indeed, The Lower Keys Hospital District indicates in its annual financial and budget statements, including the current 2016 budget statement, that it funds a “Primary Care Clinic” to the tune of $500,000 per year.
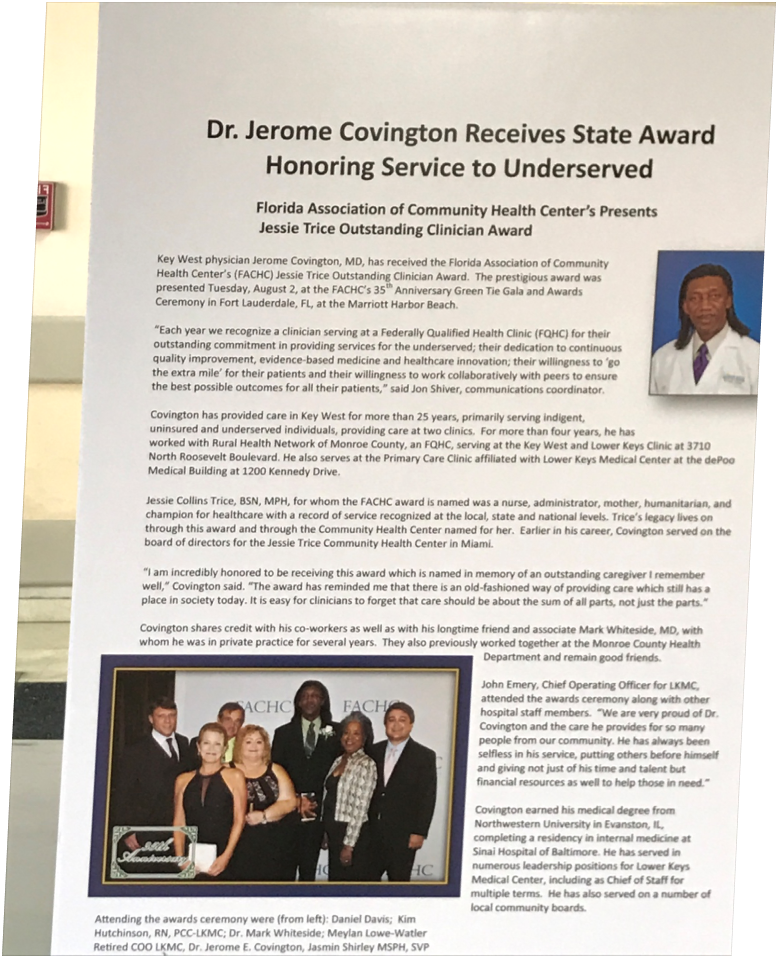
But Where is the Hospital District’s “Primary Care Clinic”? On December 1, 2016, I began surfing the Net, calling experts, talking with former employees of two Key West primary care clinics associated with the Lower Keys Medical Center, and walking and driving around Key West to locate “free” clinics listed on the Net. Looking first at the Stock Island Lower Keys Medical Center, my guess is that there is no “Primary Care Clinic” there, per se, that is operating with the help of the Hospital District funding for indigent care. Why not? The Lower Keys Medical Center’s website–in an article announcing the Florida Association of Community Health Centers’ “Outstanding Clinician Award” to Dr. Jerome Covington–stated that Dr. Covington, “serves at the Primary Care Clinic affiliated with Lower Keys Medical Center at the dePoo Medical Building at 1200 Kennedy Drive”[iii] (emphasis added).
Problem solved! It must be dePoo’s Primary Care Clinic that receives that half-million-dollar subsidy annually from the Lower Keys Hospital District for the care of indigent patients. To confirm, I called three people linked to the Hospital District: an administrator, the recently retired Chair of the District’s Board, and the Board’s lawyer: “Does the Hospital District help fund a primary care clinic at dePoo Hospital?” In no uncertain terms, each person told me in one way or another that, “we have nothing to do with that clinic.” In an email exchange with the Hospital District’s new Chair, a Blue Paper editor who asked where the clinic referred to in the contract is located was told: ‘You need to direct that question to CHS, as it is their responsibility.” What? Doesn’t the Hospital Boards’ Chair know where the contractually required Primary Care Clinic is and what the District’s $500,000 per year payment is supporting? I don’t know about you, but I keep close tabs on all of my money; I especially track the use of my money by organizations receiving my donations.
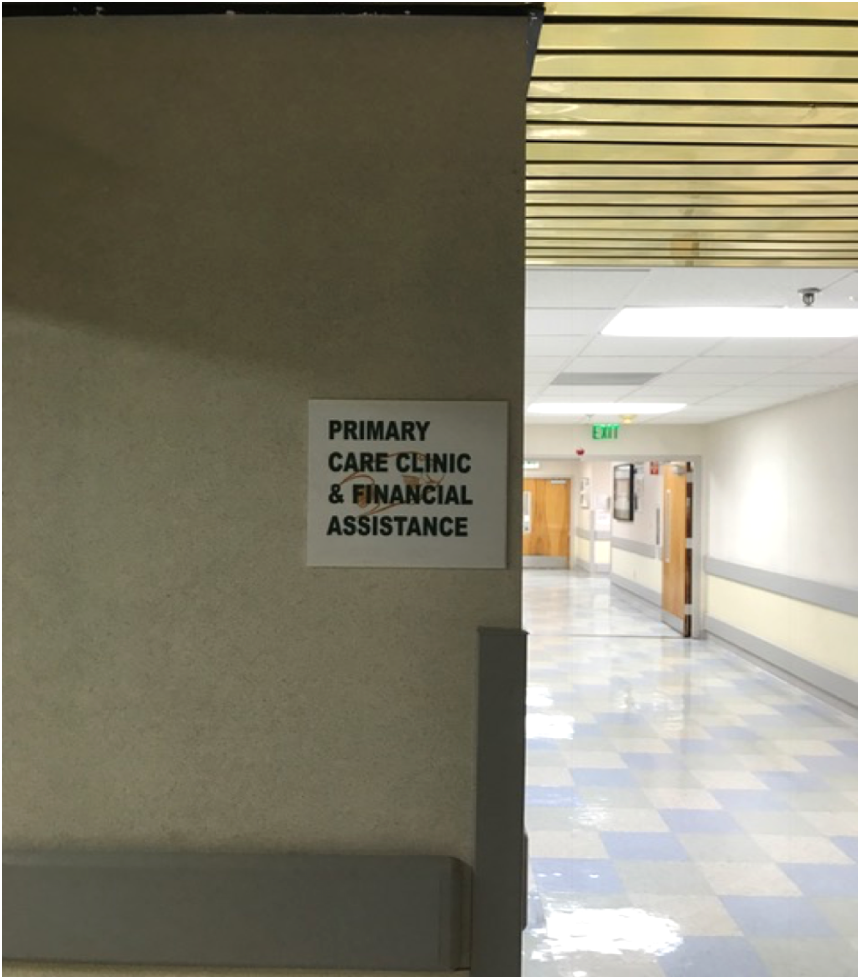
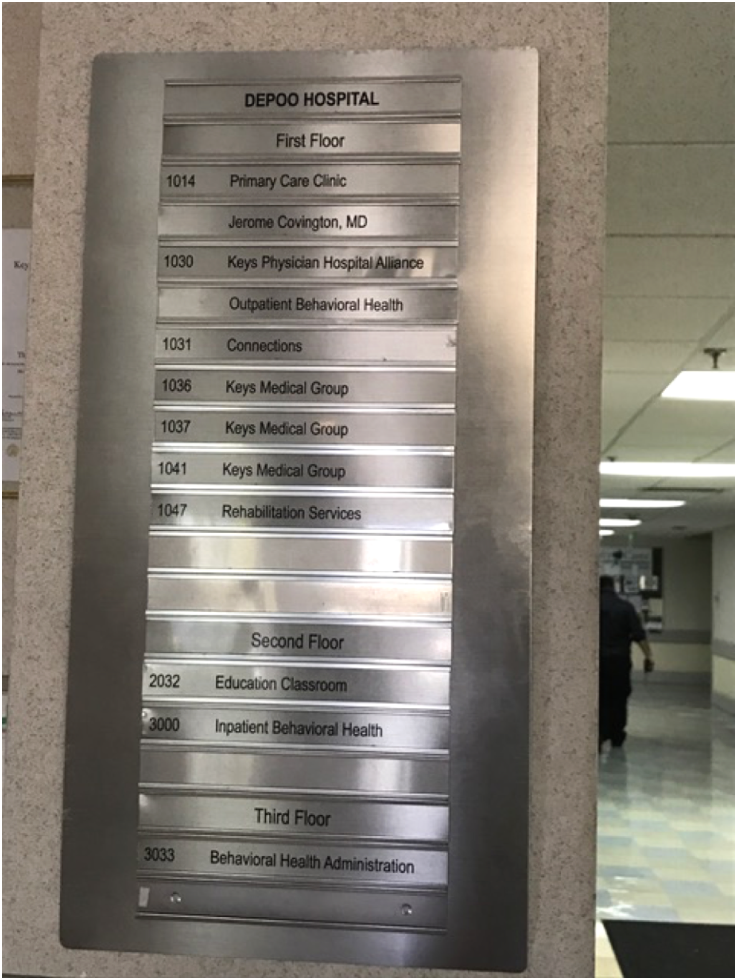 In a daze: If the Hospital District is not providing a half-million to help fund the dePoo Hospital “Primary Care Clinic,” just where is the clinic that receives that District funding? Suspecting that a ‘Primary Care Clinic’ wasn’t even operating at dePoo, I drove to 1200 Kennedy Drive to find the clinic, if it was there. A very small silver sign mounted on the entry wall just behind an apparent information desk, listed the services available at dePoo Hospital. These included a “Primary Care Clinic.” Jerome Covington, MD was listed as practicing in that Clinic located on the hospital’s first floor in Room 1014. There was no indication in the dePoo hospital lobby of the Primary Care Clinic’s hours of operation, and I was there after the hospital’s closing time so I couldn’t ask. The next day, I decided to call dePoo and ask about the Clinic’s hours. Some five telephone calls later, using each time an incorrect phone number found on-line, I finally got to a receptionist, who informed me that dePoo’s Primary Care Clinic was only open Tuesdays and Thursdays from 8am to 7pm and that the Clinic’s in-take worker helps establish a prospective client’s eligibility for free treatment. Indigents — people without financial resources or insurance to pay for their healthcare – can use the dePoo Clinic. But what about those who are underinsured and those with financial stability and insurance. My husband, with his two insurance policies – Medicare and AARP – had his ears cleaned at dePoo’s Primary Care Clinic – but that was two years ago.
In a daze: If the Hospital District is not providing a half-million to help fund the dePoo Hospital “Primary Care Clinic,” just where is the clinic that receives that District funding? Suspecting that a ‘Primary Care Clinic’ wasn’t even operating at dePoo, I drove to 1200 Kennedy Drive to find the clinic, if it was there. A very small silver sign mounted on the entry wall just behind an apparent information desk, listed the services available at dePoo Hospital. These included a “Primary Care Clinic.” Jerome Covington, MD was listed as practicing in that Clinic located on the hospital’s first floor in Room 1014. There was no indication in the dePoo hospital lobby of the Primary Care Clinic’s hours of operation, and I was there after the hospital’s closing time so I couldn’t ask. The next day, I decided to call dePoo and ask about the Clinic’s hours. Some five telephone calls later, using each time an incorrect phone number found on-line, I finally got to a receptionist, who informed me that dePoo’s Primary Care Clinic was only open Tuesdays and Thursdays from 8am to 7pm and that the Clinic’s in-take worker helps establish a prospective client’s eligibility for free treatment. Indigents — people without financial resources or insurance to pay for their healthcare – can use the dePoo Clinic. But what about those who are underinsured and those with financial stability and insurance. My husband, with his two insurance policies – Medicare and AARP – had his ears cleaned at dePoo’s Primary Care Clinic – but that was two years ago.
Whew, all is explained. Just as I felt I knew where the Hospital District-subsidized Primary Care Clinic was operating, albeit only two days a week, my “Primary Care Clinic” odyssey got complicated. Interviewing former employees from dePoo’s Primary Care Clinic, I learned that until relatively recently, the dePoo Clinic had been operated by Monroe County’s Rural Health Network (RHN)—a not-for-profit organization with county and federal funding that provides primary healthcare for rural populations. When RHN was operating dePoo’s Primary Care Clinic, the clinic went by the name, “Lower Keys Community Health Center.”[iv] As for that clinic’s connection to HMA(CHS) and the District, my interviewee stated that HMA and the Rural Health Network had, for a time, been “partners” in providing indigent care at the dePoo clinic.
Too Many Balls in the Air: Sometime in late 2014 or early 2015, the RHN re-located its “Lower Keys Community Health Center” from dePoo Hospital to 3706 N. Roosevelt Blvd., in Key West. Open Monday through Friday from 8 am to 7 pm, when one calls its phone number the caller can choose to speak and hear prompts in English, Haitian (‘Creole’), or Spanish. Jerome Covington, MD is one of its practitioners and medical director. The North Roosevelt Boulevard “Lower Keys Community Health Center,” screams accessibility, unlike the Primary Care Clinic now operating at dePoo — which is only open two days a week and frustrating to connect with by phone. My research shows that Jerome Covington’s Roosevelt Boulevard clinic—managed by the Rural Health Network—is a Federally Qualified Health Clinic (FQHC) —meaning that it qualifies for:
“enhanced reimbursement from Medicare and Medicaid, as well as other benefits. FQHCs must serve an underserved area or population, offer a sliding fee scale, provide comprehensive services, have an ongoing quality assurance program, and have a governing board of directors.”
One very well placed interviewee recalls that, dePoo Hospital and Stock Island’s Lower Keys Medical Center—both operated by HMA/CHS —regularly referred patients to Dr. Covington’s “Lower Keys Community Health Clinic” on the Boulevard. According to my source, the Lower Keys Community Health Center receives no CHS or Hospital District support or funding.
Befuddled, I asked myself: Could it be that Stock Island’s Lower Key’s Medical Center’s Emergency Room, serves in practice as the Hospital District’s Primary Care Clinic? Not according to the definition of each kind of service: Emergency Care is short-term, usually performed in an Emergency Room, such as the one at the Lower Keys Medical Center. Emergent care, as it is called, is, “Medical or other health treatment, services, products or accommodations…to an injured or ill person for a sudden onset of a medical condition.”[v] In contrast, Primary medical care is long-term. It promotes good health through on-going illness prevention and health maintenance: “A patient’s main source for regular medical care, [primary care] ideally provides… continuity and integration of health care services….[Such services] provide the patient with a broad spectrum of preventive and curative care over a period of time….” [vi]
A friend of mine had diabetes and was without either the cash or the insurance to cover his ongoing diabetes care and treatment. Without such resources, as time passed, his diabetes worsened and deep sores developed on his legs and feet. He alone could neither treat nor cure his infected wounds, so without medication, diet monitoring, and “regular foot care [to] help prevent development of severe foot sores,” [vii] my friend ended up having one of his legs amputated. This tragedy could have been avoided with on-going preventive primary care services.
Primary Care Clinic Required: The contract between the Lower Keys Hospital District and HMA, clearly includes Primary Care Clinic services for all residents in the district including the indigent, as a contractual requirement. And this stipulation was not removed by the most recent amendment: section 4 (i) of the 2003 Hospital District/HMA amendment to the 1999 contract retains language describing “primary care” as taking place in a clinic setting.
“Lessee shall maintain space for a primary care clinic (“Clinic”) at the District Hospital or dePoo Hospital, or such other location as Lessee shall designate from time to time. The Clinic shall provide a broad range of primary care health services with an expanded operating schedule to all Residents regardless of the Resident’s ability to pay.”
The 2002 Amendment: In 2002 HMA and the District amended their agreement to allow the half-million-dollar Primary Care Clinic subsidy to be used not only to pay physicians who serve indigent patients who are clients of the Primary Care Clinic, but also any indigent patient who showed up at the Lower Keys Medical Center Emergency Room for care, but who didn’t need the services of an Emergency Room physician. Hospital physicians providing care for that indigent patient – at the hospital – would now be eligible for payment via the half-million-dollar district funding, based on a finding that the care required was not of an urgent nature. HMA/CHS is required to provide urgent Emergency Room care for indigent residents; the District is no longer (since 2009) required to subsidize HMA/CHS in any way for providing state mandated hospital emergency care for indigent residents.[i]
The 2003 Amendment: In 2003 HMA and the District again amended their agreement, this time allowing the half-million-dollar funding to be used to pay physicians who treat indigent patients who are brought to dePoo Hospital under the Baker Act.[i]
No Clinic, No Half-Million: Included in the agreement (and its amendments) is the stipulation that should HMA/CHS stop providing district residents with the Primary Care Clinic described in the contract, the District would no longer be required to provide any funding including funds to subsidize hospital non-emergency treatment of the indigent coming through the ER or care for indigent Baker Act patients brought to dePoo Hospital.
“In the event that the space for the Clinic and administrative support is terminated by the lessee, then, effective upon termination, all physician services provided after termination shall not be eligible for payment, whether for services provided as a result of referral from the Clinic or the Emergency Room.” [2003 amendment]
After tireless research, I cannot say with certainty where CHS’s contractually required Primary Care Clinic [“providing a broad range of primary care health services with an expanded schedule”] is located.
Power: Alpha Dogs and Omega pooches. In providing her legal opinion, Ms. Currier limited her research and opinion, as requested, to the de jure aspects of the Hospital District/HMA contract—Do its contractual stipulations adhere to the “law, [are they] authorized by law,… [or] by statute…” Another equally pertinent way of studying contractual relations is to look at the very real day-to-day playing out of a contractual relationship: Who benefits most and least from the contract? In ‘dog pack’ language, who is the Top, Alpha Dog and who is the bottom, Omega pooch?– the lowest member of a dog pack. That question focuses on the de facto actions of the contracting parties: How does each contractual party, in fact, in reality, behave vis-à-vis the other one and toward a contract’s designated beneficiaries? Using CHS and the Hospital Disrict as the case in point, if the de Jure stipulations of a contractual relationship require that one or another party to the contract, or both, mount and operate an accessible, locatable, and affordable primary care clinic, then de facto—in fact—does such a clinic exist in the form required by its contractual description?
Perhaps the answer lies in a combination of the Hospital District’s contractual status, its psychological subservience to HMA/CHS and its willingness to let itself be uninformed about the end-uses of its $500,000 annual contribution to the Primary Care Clinic. In the words of John Padget, recently appointed Hospital District Chair, “We’ve learned that we don’t have any legal wiggle room, so let’s ask if they’re willing to amend anything.” Stating that he plans to write a “friendly letter” to Wayne Smith, Chairman of the Board of Community Health Systems and its Chief Executive Officer, Padget will cautiously ask CEO Smith: “Would CHS agree to negotiate and commit to additional operational criteria to be added to the lease as a show of good faith to the community?” And then, despite all that has gone wrong in HMA management of Stock Island’s Lower Keys Medical Center (LKMC), Mr. Padget sweetens his “friendly” deal by asking if HMA/CHS “is interested in extending the lease.” Well!
A corporate behemoth in the US healthcare industry–“CHS’ Fourth Quarter 2014 Net Operating Revenues were $4.798 Billion.”[viii] In 2014 Community Health Systems’ top executive, Wayne Smith raked in a higher compensation [$26.4 million] than all other CEOs in the healthcare provider sector.[ix] CEO Smith’s total compensation package for 2014 was almost 200%[x] more than his compensation for 2013.[xi] In contrast, in 2014, the Lower Keys Hospital District’s total net position was $10,288,694[xii] (declining almost $500K in 2015 to $9,860,378). [xiii] The Hospital District’s board members serve voluntarily—“without compensation for their services”[xiv] The largest chunk of the Hospital District’s humble revenue is derived from its investments,[xv] which can, as we know go up, or down.
‘Disappearing’ a Hospital. Using smoke and mirrors, the 1999 contractual ‘enabling act’ between the Lower Keys Hospital District and HMA effectively melded two Key West hospitals—dePoo and the Lower Keys Medical Center, located about two miles apart–into one for-profit capital asset. Only contemporary magician David Copperfield—who made the Statue of Liberty Disappear[xvi]—came close to accomplishing that feat! The hospital monopoly that has followed, greatly enhanced the value to HMA of its Hospital District asset. Having only one hospital, on paper, to serve the demographically “rural” Lower Keys, has transformed Stock Island’s Lower Keys Medical Center into a ‘cash cow.’ As last week’s Blue Paper “Editorial”[xvii] reported, the profit margins for LKMC have been as high as 32 percent of the hospital’s revenue; the US average hospital profit margin is only 7 percent. No wonder, HMA/CHS might not be interested in risking its bottom line by providing primary healthcare at low- to no-cost to the Lower Keys Hospital District’s poor and indigent. The minimalist dePoo Primary Care Clinic seems to be a functionally workable marriage: hospital profits for CHS are safeguarded, while the poor who use the dePoo clinic are minimally ‘helped’ in maintaining good health.
It’s Over When It’s Over. My research for the Blue Paper on indigent healthcare in the Lower Keys is far from finished, in fact, what I’ve written here raises more questions than answers. Most important: Is CHS using the Hospital District’s annual $500,000 dollar subsidy, ear-marked for a Primary Care Clinic, for LKMC Emergency Room and other related hospital expenses? Certainly my interviews with two former employees at dePoo’s primary care clinic, as well as a Hospital District administrator, have told me that ‘the Hospital Districts $500,000 goes to pay hospital physicians.” Well it is apparently contractually permissible for the Hospital District to allow its $500,000 in Primary Care Clinic annual funding to be used to pay for ER-sourced indigent “non-urgent” treatment and related hospital care as well as psychiatric services at de Poo hospital. However, it is not contractually permissible for CHS to short-shrift funding for a publicly accessible—open more than two days a week [!] well-advertised and locate-able, Primary Care Clinic that has an efficient plan for providing free and sliding-scale services to all Lower Keys’ residents: especially the poor, poorer, and indigent. This is precisely what is absent—and, by the looks of it — contractually mandated.
We began with our duty to help the needy and end with William Shakespeare’s reminder about law and power: King John 3:1—Constance to Cardinal Pandulph:
“When law can do no right, Let it be lawful that law bar no wrong: Law cannot give my child his kingdom here, For he that holds his kingdom holds the law.”
Happy Holidays!
~~~~~~~~~~~~~
[i] 1999 CONTRACT, 2002 Amendment, 2003 Amendment
[ii] Attorney Currier, Legal Opinion, p. 8.
[iii] http://www.lkmc.com/content/dr-jerome-covington-receives-state-award-honoring-service-underserved
[iv] http://health-centers.healthgrove.com/l/11943/Lower-Keys-Community-Health-Center
[v] http://medical-dictionary.thefreedictionary.com/emergency+care
[vi] http://www.medicinenet.com/script/main/art.asp?articlekey=5042)
[vii] Mayo Clinic explanation: http://www.mayoclinic.org/diseases-conditions/diabetes/in-depth/amputation-and-diabetes/art-20048262
[viii] http://www.businesswire.com/news/home/20160215005500/en/Community-Health-Systems-Announces-Fourth-Quarter-2015
[ix] A healthcare provider is an institution (such as a hospital or clinic) or person (such as a physician, nurse, allied health professional or community health worker) that provides preventive, curative, promotional, rehabilitative or palliative care services in a systematic way to individuals, families or communities.
[x] http://www.modernhealthcare.com/article/20150425/MAGAZINE/304259980
[xii] http://www.lfkhdb.com/uploads/files/audited_financial_statements_FY_2014_001.pdf
[xiii] http://www.lfkhdb.com/uploads/files/LFKHD_Financial_Statements_09-30-2015.pdf
[xiv] Ibid, P. 3
[xv] PFM Management, LLC oversees The District’s rather humble stock and bond portfolio.



Once again excellent reporting. WHERE IS THE FREAKIN MONEY?
Why didn’t I use that for a subtitle? “Where’s the FREAKIN money?” Thx for making my day. Martha
Follow the money and we will find the criminals. Up until recently no one questioned the contracts – we all just complained about the services, excessive costs and unfair treatment of residents and visitors to the Keys by the hospital, and our concerns were ignored all those many years. Until now, those in the past who are still benefiting financially, did an excellent job with the smoke and mirrors and convoluted contracts and documents. But slowly we will peal back the layers. Keep the heat on them Blue Paper, Ms Higgins, Harry Bethel, Judge Payne, Commissioner Kaufman, KW City Attorney, as well as the County Commissioners and Monroe County attorney (this in NOT just a KW problem – service by the hospital are provided fro those living south of the 7 Mile Bridge) and our incoming State Attorney Dennis Ward. As heat continues to be turned up, you will see a few people start to sweat. We will hopefully see some physicians and others resign and attempt to move away (though they won’t be making the kind of money they have arranged here!) – then we will know who some of the guilty parties are.
Though it may seem the more we know the more complex the situation is – this is exactly what they intended. Up until now that has worked for them. But we will not give up as a community. Their trying to play nice does not erase the past. One should never forget history. Too often the past actions predict the future.
Nice job Martha – keep digging!
There might not be any “criminals”. Just sayin’…
Dear Editor,
Thank you for your most appropriate caution! The minute we introduce such characterizations is the minute we lose…all ’round.
Martha Huggins has produced a great piece, well-articulated and well-researched…that lays out the difficulty of understanding a single facet of the Hospital “contract”…one that is easily ignored. It shouldn’t be.
I’ll be along later, as time permits, with my thoughts on the subject. Consider yourself forewarned. 😉
Dickford
It still amazes me, Naja (Editor), given the thousands of devoted blue paper readers, and the death-defying risks you and Arnaud and some of our contributing writes take, blue paper still is not even breaking even? Shameful.
Time will tell. Let’s see what Dennis Ward uncovers!
And, Naja (Editor), Dickford, there might be criminals. State Attorney-elect Dennis Ward said during his campaign earlier this year, that now out-gong State Attorney Catherine Vogel should have empanelled a grand jury to investigate the hospital. Dennis told me in an email that he thought the US Attorney should look into the hospital. The allegations of padding bills are criminal allegations. The allegations of price-gouging by a hospital management company having a monopoly are criminal allegations.
I went to the free clinic in the DePoo building, when I had scabies. The woman behind the glass told me I was not eligible for treatment, because I had Medicare; only poor people with no medical insurance could be treated there. I was not referred anywhere else.
They examined Kari Dangler at the dePoo clinic. She was indigent and had no medical insurance. However, she had to pay for her scabies prescription and be cured, before Dr. Covington arranged with a local surgeon to take Kari as a patient regarding a fistula in her colon, which was seeping into her female plumbing. And with a gynecologist. And with an anesthesiologist. And with the hospital where the surgery was done and Kari was there a week after the surgery.
But first, Covington’s office did a lot of work qualifying Kari for some kind of government funding for all of that medical care. Only after the funding was approved, did Kari see the doctors and the surgery occur. Kari received aftercare at the surgeon’s office. There was talk of her going to Dr. Covington at Rural Health Clinic for after care, but I don’t htink that never happened. I heard Dr. Covington is retiring. As I recall, after some time had passed, Kari was told by the clinic at in the dePoo building that they had to get Kari re-approved for the government funding.
I myself have seen one homeless man, known as Frisbee Dave, come into the emergency room at the hospital, with nothing of an emergency nature. He seemed to just want attention. The ER doctor greeted him, they seemed to know each other, and then told him it was not an emergency and to leave.
Across from the ER bay holding Frisbee Dave, I was in an ER bay with Kari, who was about to go crazy from the itching caused by scabies. She was close to suicidal from the itching. The ER doctor told her a skin rash was not an emergency. He said it might be scabies. He would prescribe a scabies prescription, if Kari wished. She told him to write the prescription. She’d had scabies before, caught at KOTS, and had been given the prescription for it and that had cured the infection.
Kari could not afford the scabies prescription the ER doctor wrote. She got an appointment to see Dr. Covington at the dePoo clinic. His nurse looked at Kari’s hands and the back of her legs and made her leave the reception room and wait outside on the hallway. I know this because I was there. Then, the nurse and Dr. Covington came out into the hall and both of them, from a safe distance, looked at Kari’s hands and legs, and they told her she had scabies, and that would have to be treated and cured first, before Kari could be seen by the surgeon and gynecologist.
The same prescription was written. Kari’s mother sent money. Kari bought the prescription, which is a cream with the insecticide permethrin in it. 5 percent solution. Mosquito Control Board member Steve Smith and Mosquito Control office both told me Mosquito Control used permethrin in its sprays.
The scabies infection on Kari’s feet caused her feet to look like some kind of weird animal’s feet in a horror movie. The infection on her feet was too severe and deep into the skin and tissues to be cured by the prescription. A friend of ours found a veterinary grade 10 percent permethrin solution online for about 1/6 the cost of the permethin cream Dr. Covington has prescribed. Before using it, though, Kari soaked her feet in a bucket of heavily bleaches water, 1/2 hour for each foot. Then, she poured apple cider vinegar over her feet. To kill fungus and anything else those two home remedies would kill.
It took several weeks of spraying the veterinary grade permethrin solution on Kari’s feet to obtain a cure. On the way there, she was peeling layer after layer of dead, ugly skin off her feet. Finally, she got down to pink feet. Then, she saw Covington, and he sent her to the surgeon and the gynecologist.
Before all of that, Kari had that same scabies infection the entire time she was in jail for about 9 months. The jail infirmary and its doctor, Rose Chan, M.D., refused to treat Kari, despite my finally talking with Sheriff Rick Ramsay, after I had tried to talk with Dr. Chan in the hospital cafeteria, and she said she could not discuss her patients with me, it was privileged. I said this was not about privilege, it was about the Hippocratic Oath. No it wasn’t, Dr. Chan said, angrily, and stormed off.. A flesh-boring mite, sabies is highly contagious. Dr.Chan does surgery at the hospital.She was not Kari’s surgeon.
I myself went to the ER about a year ago, one weekend, with what I was pretty sure was a young, growing MRSA lesion on my leg. The ER doctor confirmed, that wrote a script for Bactrim, a sulfa drug most preferred by doctors for new MRSA skin infections. I supposed, because MRSA has not mutated enough to defend against it. The hospital accepted my Medicare. I do not recall receiving a bill from the hospital.
Kari just now told me on the telephone that she has not received any bills from the hospital for her stay there.
Sloan, you’re getting way ahead of yourself here. Yes, of course there could be criminals. Dennis Ward can say virtually anything he wants…it’s a free country. But, it would be foolish for any prosecutor to empanel a grand jury based on the vague allegations of “price-gouging” or other financial improprieties that have been publicized. Such allegations require substantial proof just to pursue. That’s where an “investigative” grand jury can begin: Such should never be pursued as a “fishing expedition”. That’s not to say that such “proof” doesn’t exist: We just haven’t seen it.
For what it’s worth, the CHS financials point out that more than 70% of their revenue is derived from private and public insurers, Medicare, Medicaid, grants and such. I can assure you that none of those payers are slouches: Ain’t no “bill padding” there!
But, there certainly is “bill padding” when it comes to private payers without insurance: It’s common (and expected) in any hospital you care to mention. Ya’ gotta make a buck where ya’ can…this is a business, after all. But, the situation is best described as “fluid”…the patient and the hospital need to effectively communicate. This communication can be aided by means of “navigators” in the health care community. Many times, big bills can be substantially reduced…or, even completely eliminated: I’ve used this approach a few times with agreeable results.
As for any charges related to “monopoly”? Ha! Ha! Ha! You should know that there are hundreds upon hundreds of communities throughout the U.S. who have but ONE hospital. LKMC is not that different from Key West having but ONE power provider…Keys Energy. Think about it.
Anyway, we’re taking up valuable space that distracts from Martha Huggins discussion/revelations about this mysterious Hospital Board and the issues surrounding the funding of this equally mysterious Primary Care Clinic.
Let’s focus on that, eh?
Dickford
Thank you Island Girl. We continue, and thanks for your energy and efforts. Martha
The true hero in this story is Dr. Covington!! However, I have been told,after many years of service to the indigent. he will be focusing his practice on research due to health reasons. I would like to thank him for the free exams he provided my friend and prevented her from getting unnecessary surgery. His unselfish generosity is in complete contrast to the for profit CHS model. A tribute in the Blue Paper would be fitting to health care professional.
Yes gleneric, so true. There is a place for that story and it is not in this piece.
Yes, praise to Dr. Covington, whom I think I heard is an internist. Before Dr. Covington was Ian Garriques, M.D., a retired infectious disease specialist. He was the clinic doctor when the clinic was in the hospital. And he followed the clinic to dePoo building. I read a letter to the editor in the Citizen he had authored, in which he said MRSA is pandemic in the Keys. He treated me for MrSA in the summer and fall of 2003, and early 2004. He arranged surgery to save my life from MRSA. Michael Klitenic, M.D. was the surgeon. I was indigent, had no medical insurance. The hospital wrote off the bill. Years later, I came into money and paid off the old written off bill, which the business office told me I did not need to do. i told them to take my check and do for someone else what they had done for me. They took my check. I think somebody should interview Dr. Covintgon and, if he is still within contact, Dr. Garriques and hear what they have to say about the free medical clinic, as it was loosely referred to in “the old days.” I recall that Dr. Garriques had to female staff, one was a nurse, I thin the other was a bookkeeper/secretary. That was when the free medical clinic was in the hospital. People just came and were seen first come, first serve. I don’t think there were any appointments. I think that clinic was open 5 days a week. Kari Dangler had to make appointments to see Dr. Covington. A friend of mine, now deceased, said he had to make appointments, he had a really hard time getting around and was really sick, and once he went there and waited many hours and finally was seen by Dr. Covington. There was nothing Dr. Covington could have done to save my friend, and as far as I recall, my friend only went once to the clinic. He had what he called “Magellan” medical insurance, the top shelf medical insurance provided by the U.S. govnerment. My friend was medically disabled and was receiving Soc. Sec. medical disability each month, a smallish part of which was taken by the Housing Authority for his rent.
There are several requirements under the contract the District has with HMA/CHS. In exchange for a very small amount of rent, considering we are talking about a 30 year term, the company got two hospitals. Some of the rent went to the District for the LKMC [that the District owns] and some went to dePoo Hospital [privately owned]. They turned the two into one “hospital system”. So the hospital District got some rent, but in addition to very little rent they got something else: a contract that required certain valuable services: One: the company must provide “urgent” care for indigents at the hospitals as per Florida law for the entire 30 year term. For the first 10 years the District was required to “reimburse” up to $1.5 million per year for that legally required indigent care at the hospitals. The District put up 15 million immediately in an escrow account. Since 2009 the cost for this indigent care was meant to and has been borne entirely by the company. This is something they must do as part of the bargain. Two: A “Primary Care Clinic” that would give a “broad range” of primary care and operate on an “expanded schedule” and would provide the care for all residents no matter whether or not they could pay for it. The contract requires the company to provide the space and all non-physician personnel. The District is to provide “reimbursement” for payment of physicians associated with the clinic for their care of indigent patients. Over the years the use of the 1/2 million from the District was expanded as mentioned in the article. The requirement for a clinic – open to all residents on an “expanded schedule” is the issue here. The contract says that if there is no clinic as described in the contract then the District no longer needs to pay that 1/2 million to reimburse the physicians that service the indigents in association with the “Primary Care Clinic” portion of the contract. Do we have that clinic? Since the company would pay for the space and the non-physician personnel the Clinic should be at reduced cost to the community as all of the overhead is covered by the company – this again is a part of the bargain. Do we have such a clinic? It doesn’t appear that we do and the Board members in charge appear to be telling us they don’t know anything about it – and we should go ask the company if we want to know… Next phase is to find out exactly how the 1/2 million is being spent. I don’t expect this will be easy. Stay tuned.
Looks to me like the next step is to ask Governor Scott to fire the Hospital Board, which will be a waste of time. So the next step is to shanghai the Hospital Board and take them out to sea and feed them to the sharks.
Looks like the first step was to interview Dr. Covington, and, if he could be found, Dr. Garriques.
Last time I was at the indigent medical clinic in the dePoo building, maybe a year ago?, Dr. Covington was running it. It was open a couple of days a week.
C’mon, Sloan! I realize that you’re trying to inject a li’l wry humor into this discussion, but really…is it necessary?
Both Martha Huggins and our Dear Editor Naja have provided us with a wealth of detail from which we can develop the pertinent questions -and- hopefully, get reasonable answers:
1. Just WHERE does this “Primary Care” facility actually exist? Don’t just say “DePoo” or “the hospital”. What floor? Room (or suite) number?
2. What is the contact phone number for this facility? What are its hours of operation? Which days?
3. Does the Hospital Board itself maintain a contact phone number, email account? Does it maintain a staff of any kind?
4. Now, we’re down to the nub of the matter, in my opinion: To whom EXACTLY is this quarterly stipend of $125k paid? Is there any accounting for this expenditure? As I understand it, this money was to be used for the primary purpose of paying for the services provided by medical doctors — exclusive of the costs of any supporting staff and facilities, which are to be provided by HMA/CHS. I could be wrong in my interpretation. But, if that is essentially true, I find it implausible that these doctors cost a half million bucks a year. Especially, if this “clinic” is only open two days a week.
That’s just for starters…
Dickford
Dear Sloan, why don’t you interview Dr. Covington. He will be part of one of my stories at some point, not here. I will be happy to have your interview of him, martha
This is your project, Martha. You should have interviewed Dr. Covington, since he is the primary care indigent clinic doctor. The primary care clinic is what your article is about. You also should have tired to track down and interview Dr. Garriques, who preceded Dr. Covington at the primary care medical clinic,which we used call the free medical clinic, since it was for poor people.
You might nor might not care to know, Martha, Dickford, Naja, etc., but Arnaud came to me in a dream before dawn today, mimicking a gorilla jumping up and down, inviting me to do same with him. So just naturally I had to head to the blue paper to see what that might be about and here it is.
Martha, I know a bit about investigative journalism. I tend to do it by wallowing in the subject matter, Such as, going to medical clinics and being treated and reporting that. By sleeping at the city’s homeless shelter and reporting that. By eating at the soup kitchen and reporting that. By talking with lots of homeless people, and reporting that. By sleeping nights in the police station lobby and reporting that. By attending city commission meetings and pissing off the mayor an d commissioners with my citizen comments, and reporting that. By challenging police officers in the field, and reporting that. Also, I lived a year in Arnaud and Naja’s home and saw, heard what they go through, and talked plenty with them about that, trying to get to the bottom of things. All the people they can’t get to put their faces and names on what they want exposed.
You need to interview Dr. Covington. It’s nuts that you say that is for me to do. You also need to try to interview Dr. Garriques, if he is sitll alive and can be found. They, Mart ha, are the medical horses’ mouths for the primary care indigent medical clinic.
Actually, I meant what I wrote, Dick. The Hospital Board has been asleep at the switch, basking in its own self importance. They all should be dismissed.
Naja and I talked about 2 days ago, at her and Arnaud’s home.
About an email Naja sent to Jill Cranney, who is an elected Mosquito Control Board member, paid, who is a paid administrative aid for the Hospital Board, asking for information about the free clinic – Please acknowledge receipt of this email, Naja said she wrote to Jill. Up to 2 days ago, nothing back from Jill, whom I told Naja I have heard makes her living being on boards or working for them.
I happen to be a user of the hospital, and know people who are. I have been a user of the free clinic, and know people who are, and I know right were it is, as do most poor people in Key West.
I personally have gotten terrific treatment at the free clinic, and at the hospital. But it’s been a while since I was treated at the free clinic, and its days of operation are now reduced.
Key West Island Girl (Christine Russell, who is gung ho to spank the appointed hospital board and the hospital management company, prosecute CHS, goes to Panama to get medical treatment.
Naja told me 2 days ago, if she or Arnaud d a serious medical problem, they would go to Martinique or Guadaloupe, in the Windward Islands – French colonies, where there is superior and much cheaper medical treatment. Arnaud went there a few years ago to be treated for MRSA.
I told Naja 2 days ago, Martha Huggins should have interviewed Dr. Covington for her article; Martha blew the assignment, when she did not do that.
There certainly is plenty of information in Martha’s article, which raises many questions for which, so far, there are no good answers. Dr. Carmichael was the person to start with, though. He runs the free clinic in dePoo. I have heard he is the doctor at Rural Health, too.
From what I heard from Kari about how Dr. Covington and his office staff went about treating Kari at the dePoo clinic, and getting her treated by private doctors and having surgery in the hospital, I got the impression Dr. Covington knows a great deal about what is going on with the free clinic and its funding, or lack thereof.
Dr. Covington dressed the city commission and citizens down at the town hall meeting for criticizing the hospital BEORE it was farmed out to HMA.
I very much would like to see an interview with Dr. Covington reported in the blue paper. And with Dr. Garriques, if he can be found.
Sloan,
RE: The Hospital Board has been asleep at the switch.
Maybe. We’ve heard literally nothing about their activities. You mention Jill Cranney-Gage as being a paid administrative aide for the Hospital Board. Yet, where is the confirmation of such? I can find no evidence that any administrative staff is being paid for by the Board.
You claim that you KNOW where this clinic is…as do many other indigent souls. What is this? Some big “secret”? EXACTLY where is this facility? Why not share with us all here with the answers to the pertinent questions? Names, location(s), phone numbers…please!
I don’t qualify for care at this clinic…but, like you, I have received excellent care at LKMC under both HMA and CHS. My out-of-pocket costs were nominal…a coupla hundred bucks at most. Both times I was routed to specialized care at hospitals on the mainland…where I was treated very professionally (and effectively) at virtually no cost to me. Navigators were available every step of the way…guiding events to a caring recovery. Even the food was good. 😉
So…my question remains: Just what are we all bitchin’ and moaning about? Why on earth would the City “want its hospital back?”
Martha Huggins raises material questions with regard to the operations of the Hospital Board. Essentially, just how is the money handled for this “Primary Care” facility? From what I can see, the Board now cuts a check to (presumably) CHS once a fiscal quarter for $125k…which (I’m guessing here) is meant as an offset to the monies laid out by CHS to underwrite the activities of this “secret clinic”. If that proves to be true, then this Board is sloppy, to say the least.
Finally, “dismissing” the Hospital Board…even if it were a possibility, would prove nothing. Don’t start with this “repeal and replace” nonsense that is popular today: The net effect of such an effort will surely drown any benefits that were previously available.
John Padget has laid out a tentative plan to try to get everyone to work together to iron out the various issues. I favor this course…at least for now.
Dickford
The Hospital District has a website, though not entirely up to date in terms of officer titles, you will find information regarding who is on the board and who works for the board [attorney, accountant, administrator] and you will find financial documents. The administrator position is a part-time job. Have fun… http://www.lfkhdb.com/
As stated in the article: via amendments in 2002 and 2003 to the portion of the contract dealing with the “Primary Care Clinic” the use of the money for physician services outside the “clinic” both at LKMC and at dePoo became another acceptable way to use the 1/2 million per year furnished by the District. The contract states that in order for the $125,00 per quarter to be paid by the District to reimburse physicians there must be a clinic that is open to “all residents” on an “expanded schedule” — that includes you and me. The money is paid to a company – an alliance of physicians – the company is tasked with making sure the Clinic has enough physicians signed up to take care of indigents and of paying the physicians for the care. They are paid a fixed sum which is later justified and which can be reduced or increased for the next period depending on the actual services rendered in the prior quarter. The contract also states that if there is no clinic then not only is there no more money for physicians serving indigent patients at the clinic but there is no more money for the physicians who serve indigents, who come to the ER for non-urgent care at LKMC or for psychiatric care at dePoo, and are eligible for a portion of the 1/2 million pursuant to the 2002 and 2003 amendments. Assuming the clinic at dePoo that three District officials said the District has ‘nothing to do with’ is “the Clinic” then the question becomes: does that Clinic suffice? If it is only open only 2 days a week, if it only serves SOME residents instead of ALL residents as is called for in the contract — does that constitute a material breach of the contract? Disturbing is the fact that board members are not asking these questions. They are paying but claim not to even know where the Clinic is — ‘it is not their responsibility’… Then there’s this: The company [now CHS] must provide free indigent care for residents – this is required by law that allowed the District to enter into this lease. Providing free indigent care to residents is a Hospital District duty and is a condition of the contract with HMA/CHS. Since 2009 HMA/CHS have not had any help paying for this “urgent” indigent care. [The district paid $15 million over 10 years.] The half-million for primary care is being used, in part, to pay doctors at the LKMC to take care of indigents who come to the ER. I’m not sure that we will be able to get there because of HIPPA laws, but it would be interesting to see how the company is taking care of indigents who show up at the ER — both in “urgent” cases and in “non-urgent” cases. And how the 1/2 million is being spent.
Excellent response, Dear Editor! You’ve boiled it all down to the question originally posed by Martha Huggins, to wit: How is the (annual) $500k stipend being spent?
Thank you for the link to the Hospital Board’s website: The [Financial] button brings us to their 2015 Annual Report…which provides a wealth of information, if you can wade through all the verbiage and boilerplate. Essentially, the “history” of the “Primary Care Clinic” evolves into the present day practice of paying out this $500k annual stipend to this “alliance of physicians”…and NOT to CHS directly, for services rendered in service of the requirements outlined in this lease agreement.
What is needed here is a clear definition of terms: A truly indigent individual has NO ACCESS to financial resources and would entitle such persons to be treated under the auspices of the agreement. However, people with access to CHIP, Medicare/Medicaid, insurance (private or public) should be shunted to the many private providers available.
The ER at LKMC must provide services that qualify…to anyone. That does NOT mean that it is free. Many indigents are provided quality care…the cost of which is billed to Medicaid. As you might surmise, Medicaid pays for such at its own schedule of rates…leaving a “hole” in the revenue that CHS expects. Not an unexpected outcome.
Let’s face the fact that HMA/CHS is a business…a profit-oriented enterprise.
That said, to get back to Martha Huggins original question…let’s spend our time and resources figuring out EXACTLY how the funding for this “Primary Care Clinic” is expended. And, no…there should be no HIPAA restrictions on these efforts. Who got paid? How much? We shouldn’t care who the actual clients were.
Dickford
Dear Dickford, thanks for the input. I read all CAFR (financial reports). Love reading them, really. they are my go-to —look-there-first–data. We are getting there with the research, much more to come. Martha
As for difficulty getting people to talk: I called carney- several times and no one answered so I left a message for her to call (using my 518 area code). No call back so then I called using my home phone (local area code) and she answered. Absolutely NO ONE answered by calls. That’s combat-level research. You have no idea Sloan what investigative reporters have to do to get their information Martha
Heh! I second your comments, Martha vis-à-vis “what investigative reporters have to go through…”
Just imagine what the common, ordinary consumer is faced with!
WRT your previous message, yes…I am quite comfortable delving into financials. Yet, I know that most other folks are not. I fear that this is where most of this enmity we’re seeing originates.
Yes, there are issues with LKMC…not unlike the very issues we face with Sears, Comcast, FKAA…you name it. Each gets resolved in its own way and timeframe.
I can say that financial issues I had with LKMC were readily resolved to my satisfaction. No, I am not an apologist for LKMC or CHS…but, if they are willing to pay me a stipend, I would be happy to provide my receiving particulars. 😉
That said, your original question(s) have not been adequately answered, IMO: It’s unfortunate that the Hospital Board has (apparently) no public access. That should be addressed immediately…if not sooner.
Still…I can see no “criminality” here. Nor, any malfeasance, for that matter. Can these organizations do better? That’s a rhetorical question.
Dickford
Dickford, I can’t say I seen any ciminality – yet – in what Martha researched and reported about the indigent primary care medical clinic. Unless bills are being padded. Medicare is being over- charged.stuff like that. However, Key West Island Girl (Christine Russell), in comment 3 under this article, in her first sentence, made criminal allegations, and while that went beyond, perhaps, what’s in Martha’s article, it addressed genuine concerns about CHS way of operating the hospital generally, which cannot reasonably be expected to set aside, as if they do not even exist, when discussing an article such as Martha’s. If the beast is laced with corruption at the hospital, it reasonably can be though corruption consumes the entire beast.
Sloan, see what I mean? Once you focus on Martha’s questions, things fall into place. You’re making the claim that dePoo is the place — where this ephemeral “indigent primary care facility” is located. Fine! What are its hours of operation? What days are they open? Do they have a contact phone number?
You know as well as I do that whatever allegations Ms. Russell has leveled WRT Medicare/Medicaid billing irregularities by HMA/CHS are NOT pertinent to this discussion. Indigent people are exactly how they’re described — entirely bereft of financial resources: That includes Medicare/Medicaid.
You also liberally use the biggest word in the English language: IF. “IF the beast is laced with corruption…”. Is it?
Ms. Russell’s piece correctly described past cases against CHS…cases which saw that outfit settle for nearly $100 million in claims related to actions ending in 2010…and NOT related, in ANY way, to LKMC. Please note that this was a civil settlement that did not entertain any liability (or criminality).
These “genuine concerns” of which you speak belong to last week’s article…not Martha’s article.
Let’s keep things straight, eh?
Dickford
Dickford, when I was with Naja and Arnaud the other day, Naja looked at the Hospital Board’ website and pretty quick found Jill Cranney-Gage (apologies for leaving out Gage in my earlier reply, I had it in, then corrected something and dyslexed out Gage), is being paid about $10,000 a year by the Board. Naja was flummoxed (I could also say pissed as hell), that she had heard nothing back from Cranney-Gage. I still say the Hospital Board should be sacked. Put Naja and Christine Russell on it. I can provide quite a few names of local people I doubt would have fallen asleep at the switch; who would have been poking and digging and pissing people off the entire time the were on the Hospital Board. But then, who wants those kind of people on a hospital board? Or in any important public position?
Based on what all I have experienced and seen go down at the hospital ER room, and in visits to poor friends in hospital rooms, the hospital is providing a lot of care to indigent people, but that is not “primary” care; ie., ongoing, readily available (as in regular working days) treatment for medical problems. Getting the free clinic back to where it once was might prove a steep road, but I hope the blue paper is able to ignite that result. I still say the 2 indigent clinic doctors, Covington and Garriques, need to be interviewed and the results of those interviews reported in the blue paper.
If, in fact, CHS has mended its errant, money-grubbing, screw you Key West and the lower Keys ways, then I agree with you, Dickford, why get rid of CHS? I do not and never will agree with you, though, that the allegations of padding bills and price-fixing (gouging) should be allowed to die for want of one of the available 800 pound gorillas, the State Attorney, the US Attorney, the FBI, the US Department of Justice, thoroughly investigating those allegations and, if there is substantive evidence of wrongdoing, and the $ amount is substantial, criminal prosecution should proceed, just as it proceeded, hmmm, against Superintendent of Schools Randy Acevdeo and his thieving wife and subordinate, Monica, whom he tried to protect by doing nothing after he was apprised of what she was doing.
Dennis Ward prosecuted them both, and for doing it, and for prosecuting the son of save-the-hospital city commissioner Harry Bethel for robbing lobster traps, and for prosecuting other Key West Conchs and their relatives and friends, Ward was beaten by Catherine Vogel in 2012, because of the huge vote against Ward in Key West. Will Ward follow through on his campaign rhetoric earlier this year, that a grand jury should have been convened by Vogel to investigate the hospital? Will Ward follow through on his statement to me in an email earlier this year, that the US Attorney should investigate the hospital under CHS management? Time will tell.
The poor people’s primary care clinic is: first, the clinic in dePoo building; second, Rural Health on North Roosevelt Blvd, if they can get an appointment there; anytime, the ER room at the hospital, which many poor people use like a doc in a box office.
Sloan, again you’re confusing issues.
First, of course “many poor people use the ER room like a doc-in-the-box”: When ya’ hurt, ya’ go where they take care of such things. I can’t recall where I’ve ever seen folks actively looking for “health care alternatives”. Have you?
Yes, you claim that this “Primary Care Clinic” does exist…yet you refuse to publish its exact location within DePoo hospital…who to see…hours of operation…telephone number, or anything else. What’s up with that?
And, no…the Rural Health Network has a mission separate and apart from any requirements posed under this “Primary Care Clinic”. As far as I know, they receive NO funding from the Hospital Board.
C’mon! Put your “legal beagle” hat on for a moment. You might find it refreshing. 😉
Dickford
Dickford, it’s the mecial clinic run by Dr. Covington in the de Poo building, Go to that building, ask anyone who works int he building where the clinic is. Then let your feet take you there. Like my feet and Kari’s feet took us there.
I personally have seen people go to the ER room, and I have done it, instead of a doc in the box, for things the ER room would not view as an emergency. it happens.
I don’t have to prove anything to you, Dickford. I did what I describe. I saw others to it.
Sloan, no you don’t have to prove anything to me. But, you should provide the information I asked for to your many, faithful readers. It’s only the right thing to do.
I know that you’re either cognizant of the facts or can find them out. The questions are simple: Where in dePoo is this clinic? What are its hours of operation? What days? What’s their phone number?
Those questions dovetail into what both you and I have observed: People DO go the ER to address issues that clearly are NOT “emergency care”. Why? Simple…that’s the only place they can think of that is open and available. So…I ask again: Share your knowledge of this clinic in dePoo. Is that too much to ask?
Personally, I’m aware that I do NOT qualify for the services of this clinic, though I might WRT the Rural Health Network (RHN): I have Medicare and Medicaid.
Dickford
Curious, Dickford, as to why you would say that you do not qualify to use the services of the Clinic in question. To me the contract describes, a Clinic for All Residents. Physicians when servicing the indigent are paid by the District. This does not mean that the Physicians can not be paid thru other insurance (govt or other) for services provided to Residents who are not indigent. I believe the Contract describes a requirement for a Clinic that provides a broad array of primary care for all residents and that it should be open on an “expanded schedule”. Apparently the two day a week Clinic at dePoo is what is being provided and apparently (to be confirmed) they serve ONLY the indigent but that is NOT what is described in the contract and amendments that have been provided. I agree that it is disturbing that the Hospital Board has no answers. Asking past and current Doctors who provide services at the clinic, as Sloan suggests, would answer some of your questions but not questions about how the Hospital District board is overseeing the company’s adherence to contract provisions. My emails (first one dated Monday December 19th) asking for access to public records have yet to be so much as acknowledged by the Hospital
District’s paid administrator.
Not sure I agree that HMA/CHS is exempt from public records requirements just because it is a private entity. See AG opinion:
http://myfloridalegal.com/__85256236006EB5E1.nsf/0/8D4CED458D275068852564E900526C8A?Open&Highlight=0,public,records,contractor
After a Court came up with a ruling in line with this attorney general ooinion and the jurisprudence it points to – about a hospital leased to a private company by a Hospital District like ours, our Florida Legislators amended the statute allowing these leases and simply wrote a few more sentences declaring that the companies are not subject to the public records act and that the leases may not be construed as a delegation of the District’s powers – no matter the facts or the circumstances. Apparently this legislation has not been challenged…
Dear Editor,
No…this legislation has not been challenged. But, that fact implies something that is also not true: CHS is indeed subject to a WIDE panoply of public examination…by state and federal regulators. CHS is a PUBLIC company…not privately-owned. Their finances -and- their operations are subject to the scrutiny of many governmental authorities. See “keywestislandgirl” below for an example.
Dickford
There are so many pieces to this puzzle, and yes the point of Martha’s latest article seems to be a mysterious “Primary Care Clinic”. I think the whole hospital scheme was set up many years ago intentionally so convoluted, so that no one could easily unwind the strings – but to follow the money that will lead to what I referred to as some criminals. Since there was some discussion about if there are any criminals, I had to further comment.
As a member of the Committee To Rescue Our Hospital (CTROH) – I, other members of the committee, and the media – all received dozens, probably more than a hundred emails of patients complaining (and these probably only a fraction of those who were treated so badly) who are totally disgusted with the health care they received (or did not receive) and or the grossly excessive costs of procedures and care. I think someone talked about medical care costs being out of control throughout our country – Amen to that! But what we have at LKMC is something different.
I read the many stories and complaints of people who were quoted the cost of procedures and how much they needed to bring to pay (often times told to bring CASH) and upon arriving for a procedure the the amount of cash they were required to pay at the time rose excessively – sometimes ten fold! And procedures LKMC would charge $4000 – $5000, they were available at other licensed medical facilities for $200 – $300. I think there IS something criminal going on when I read the many accounts which I have over the past year, but also the many sad stories I have heard first hand over any years.
But there be bigger problems for CHS here in Key West down the road and this saga continues. Are you familiar with the Stark Law?
When someone earlier mentioned Medicare and Medicaid, I recalled this is where there could possibly be (ANOTHER) big legal problem for CHS. Maybe CHS and others can try to cheat the innocent citizens in our community of their hard earned money, but NOT the US government! Maybe you would like to read a little more : “Community Health Systems Inc. to Pay $98.15 Million to Resolve …
https://www.justice.gov/…/community-health-systems-inc-pay-9815-million-resolve-
Aug 4, 2014 – Community Health Systems Inc. to Pay $98.15 Million to Resolve False … The Stark Law prohibits a hospital from submitting claims for patient ….”
Maybe another idea for Martha and The Blue Paper to consider and investigate!
Dear keywestislandgirl,
You’ve obviously studied this issue. Bravo! You mention the “Stark Law”. Please note that it applies only to Medicare/Medicaid claims. And, even at that, it provides only civil awards and penalties…nothing criminal.
As for the cases against CHS (and HMA), please note that the activity in question occurred before 2010…six years ago. And…they occurred in OTHER regions of the country…not (apparently) in Key West. This agreement was executed before CHS even acquired HMA.
As for all the complaints that CTROH has fielded thus far…how many have produced palpable, credible evidence? And, as for if folks arrived for a procedure where the price “LKMC would charge $4000-$5000, where they could get a similar procedure for a tenth of that cost”…what precluded them from availing themselves of the less expensive procedure?
My question to CTROH remains: Assuming the City COULD take back their hospital…WHAT would they do with it? Still…no answer. [sigh]
Oh, yeah…since you might be thinking of attracting Baptist Health Systems, remember that they, too…have been censured under the Stark Law.
Finally, let’s never forget that our current governor was required to pay over $300 million as part of the $2.1 billion settlement with Columbia/HCA…a record, in its day.
Yes, I’ve heard as many complaints about LKMC as you have. I have also heard as many praises of the care at this facility under both HMA and CHS. In fact, I have been treated there under both administrations…with very satisfying results, both physically and financially.
In sum, I challenge CTROH to either put up or shut up.
Dickford
Just to address one issue from the above post by keywestisland girl. The entire medical industry in this country is messed up. Here in Ohio I have had to pay some money up front before a procedure is performed. I have found in the past that I was charged for a pain pump which I never had and the insurance company did not care. Twice I was told my out of pocket charge would be one thing and then after the procedure they tried to charge me 3 times the amount. By going through the Ohio Attorney General Office they just forwards messages to the opposing parties. I won both cases. I even lectured the OAGO attorney on the law but it made no difference. Yes, every branch of medicine in this country is f***ed up but probably more so in KW.
Bozewell,
RE: The entire medical industry in tis country is messed up.
Truer words were never said! So…what can we/should we do? You provided a strong answer by your own situation…one that is available to most of us.
I have resorted to use of this mechanism myself…in the Keys (involving Fishermens’ Hospital, not LKMC). The issue was satisfactorily resolved forthwith.
Things should NOT be this way for folks…but it is what it is. It’s a damned shame, in my opinion.
Dickford
Here in Ohio a Hospital Price Disclosure legislation is up for review and the medical industry is lobbying against it. Basically it states that a patient should know his out-of-pocket cost upfront if the procedure is a standard procedure. The medical industry is against it so they can take advantage of those who are ill informed, not informed or just do not care. With mass media and more informed citizens we somehow allowed greed to grow and become more stronger than the health of our nation. In the case of KW, keep supporting the Blue Paper and keep bitching to make things better and at least LEGAL. You need people with a Brain, some Balls and the intelligence to spot and fix these problems. You’ve got them down there. Who cares if they f++ked up years ago. Make up an integrity test and push them to run.
Bozewell,
Valid points all the way around! Can’t disagree with a single thought!
But…I’ll interject a few thoughts of my own:
– Most consumers can get an idea of what their procedures will cost…if they only think to ask. In many situations, that is not surprising…it certainly is not the most pressing question on one’s mind.
– Undergoing any medical procedure is quite unlike any other experience on our lives: We certainly cannot equate it with gettin’ the ole jalopy fixed. Even with seemingly trifling ailments, unforeseen complications can rear their ugly heads.
But, your points are well taken. In my own personal experiences with LKMC, I can truthfully state that I had no issues whatsoever. Obviously, others claim otherwise.
We shall see.
Have a Happy New Year!
Dickford
Blue Paper – Might you include the entire opinion from the Dept of Justice that I referred to in my above comment? I think your readers would find this very revealing as to CHS’s ethics and legal problems!
Department of Justice
Office of Public Affairs
FOR IMMEDIATE RELEASE
Monday, August 4, 2014
Community Health Systems Inc. to Pay $98.15 Million to Resolve False Claims Act Allegations
The Justice Department announced today that Community Health Systems Inc. (CHS), the nation’s largest operator of acute care hospitals, has agreed to pay $98.15 million to resolve multiple lawsuits alleging that the company knowingly billed government health care programs for inpatient services that should have been billed as outpatient or observation services. The settlement also resolves allegations that one of the company’s affiliated hospitals, Laredo Medical Center (LMC), improperly billed the Medicare program for certain inpatient procedures and for services rendered to patients referred in violation of the Physician Self-Referral Law, commonly known as the Stark Law. CHS is based in Franklin, Tennessee, and has 206 affiliated hospitals in 29 states.
“Charging the government for higher cost inpatient services that patients do not need wastes the country’s health care resources,” said Assistant Attorney General Stuart F. Delery for the Justice Department’s Civil Division. “In addition, providing physicians with financial incentives to refer patients compromises medical judgment and risks depriving patients of the most appropriate health care available. This department will continue its work to stop this type of abuse of the nation’s health care resources and to ensure patients receive the most appropriate care.”
The United States alleged that from 2005 through 2010, CHS engaged in a deliberate corporate-driven scheme to increase inpatient admissions of Medicare, Medicaid and the Department of Defense’s (DOD) TRICARE program beneficiaries over the age of 65 who originally presented to the emergency departments at 119 CHS hospitals. The government further alleged that the inpatient admission of these beneficiaries was not medically necessary, and that the care needed by, and provided to, these beneficiaries should have been provided in a less costly outpatient or observation setting. CHS agreed to pay $89.15 million to resolve these allegations. The settlement does not include hospitals that CHS acquired from Health Management Associates (HMA) in January 2014.
In addition, the government alleged that from 2005 through 2010, one of CHS’s affiliated hospitals, LMC in Laredo, Texas, presented false claims to the Medicare program for certain cardiac and hemodialysis procedures performed on a higher cost inpatient basis that should have been performed on a lower cost outpatient basis. The government also alleged that from 2007 through 2012, LMC improperly billed Medicare for services referred to LMC by a physician who was offered a medical directorship at LMC, in violation of the Stark Law. The Stark Law prohibits a hospital from submitting claims for patient referrals made by a physician with whom the hospital has an improper financial relationship, and is intended to ensure that a physician’s medical judgment is not compromised by improper financial incentives, and is instead based on the best interests of the patient. CHS agreed to pay $9 million to resolve the allegations involving LMC.
“This is the largest False Claims Act settlement in this district and it reaffirms this office’s commitment to investigate and pursue health care fraud that compromises the integrity of our health care system,” said U.S. Attorney David Rivera for the Middle District of Tennessee. “This office is committed to ensuring that all companies billing government healthcare programs are responsible corporate citizens and that hospital providers do not engage in schemes to increase medically unnecessary in-patient admissions of government healthcare program beneficiaries in order to increase profits.”
“This settlement demonstrates our commitment to working with our law enforcement partners and with the Department of Justice to protect the integrity of our nation’s health care system,” said U.S. Attorney Kenneth Magidson of the Southern District of Texas. “Put simply, these types of fraudulent practices will not be tolerated and the investigation and resolution of such claims will continue to be a high priority of this office.”
“Health care providers should make treatment decisions based on patients’ medical needs, not profit margins,” said U.S. Attorney Anne M. Tompkins for the Western District of North Carolina. “We will not allow this type of misconduct to compromise the integrity of our health care system.”
As part of today’s agreement, CHS entered into a Corporate Integrity Agreement with the U.S. Department of Health and Human Services – Office of Inspector General (HHS-OIG), requiring the company to engage in significant compliance efforts over the next five years. Under the agreement, CHS is required to retain independent review organizations to review the accuracy of the company’s claims for inpatient services furnished to federal health care program beneficiaries.
“In an effort to ensure the company’s fraudulent past is not its future, CHS agreed to a rigorous multi-year Corporate Integrity Agreement requiring that the company commit to compliance with the law,” said Inspector General Daniel R. Levinson, of the U.S. Department of Health and Human Services. “The dedicated work of OIG’s investigators, auditors, and attorneys, in concert with our law enforcement partners, has again resulted in the recovery of taxpayer dollars and better protection against fraud in the future.”
The settlement resolves lawsuits filed by several whistleblowers under the qui tam provisions of the False Claims Act, which permit private parties to file suit on behalf of the government and obtain a portion of the government’s recovery. Those relators are Kathleen Bryant, former Director of Health Information Management at CHS’s Heritage Medical Center in Shelbyville, Tennessee; Rachel Bryant, former nurse at CHS’s Dyersburg Hospital in Dyersburg, Tennessee; Bryan Carnithan, former Emergency Medical Services Coordinator at CHS’ Heartland Hospital in Marion, Illinois; Amy Cook-Reska, former coder for CHS’ LMC in Laredo; Sheree Cook, former nurse at CHS’s Heritage Medical Center in Shelbyville; James Doghramji, former internal medicine and emergency room physician at CHS’s Chestnut Hill Hospital in Philadelphia; Thomas Mason, former emergency room physician at Lake Norman Regional Medical Center in Mooresville, North Carolina; Scott Plantz, former emergency room physician at CHS’s Longview Regional Medical Center in Longview, Texas; and Nancy Reuille, former nurse and Supervisor of Case Management at CHS’s Lutheran Hospital in Fort Wayne, Indiana. The relators’ share of the settlement has not yet been determined.
This settlement illustrates the government’s emphasis on combating health care fraud and marks another achievement for the Health Care Fraud Prevention and Enforcement Action Team (HEAT) initiative, which was announced in May 2009 by Attorney General Eric Holder and the Secretary of Health and Human Services. The partnership between the two departments has focused efforts to reduce and prevent Medicare and Medicaid financial fraud through enhanced cooperation. One of the most powerful tools in this effort is the False Claims Act. Since January 2009, the Justice Department has recovered a total of more than $20.2 billion through False Claims Act cases, with more than $14 billion of that amount recovered in cases involving fraud against federal health care programs.
This settlement was the result of a coordinated effort by the U.S. Attorney’s Offices for the Middle District of Tennessee, Southern District of Texas, Northern and Southern Districts of Illinois, Northern District of Indiana and Western District of North Carolina; the Civil Division’s Commercial Litigation Branch; HHS-OIG; DOD’s Defense Health Agency – Program Integrity Office and the FBI.
The lawsuits are captioned United States ex rel. Bryant v. Community Health Systems, Inc., et al., Case No. 10-2695 (S.D. Tex.); United States ex rel. Carnithan v. Community Health Systems, Inc., et al., Case No. 11-cv-312 (S.D. Ill.); United States ex rel. Cook-Reska v. Community Health Systems, Inc., et al., Case No. 4:09-cv01565 (S.D. Tex.); United States ex rel. James Doghramji; Sheree Cook; and Rachel Bryant v. Community Health Systems Inc., et al., Case No. 3-11-cv-00442 (M.D. Tenn.); United States ex rel. Mason v. Community Health Systems, Inc., et al., Case No. 3:12-cv-817 (W.D.N.C.); United States ex rel. Plantz v. Community Health Systems, Inc., et al., Case No. 10C-0959 (N.D. Ill.); United States ex rel. Reuille v. Community Health Systems Professional Services Corporation, et al., Case No. 1:09-cv-007RL (N.D. Ind.). The claims resolved by this agreement are allegations only and there has been no determination of liability.
14-822
Civil Division
Updated September 15, 2014
For those who keep saying “there’s no crime,” Huggins never even hinted that there is one. We are looking at possible contract violations martha
Martha, thanks for the clarification on that point: No, you never did hint that any crime existed. However, that is quite different from several others here who claim the opposite…even to clamoring for federal investigations and grand juries.
Perhaps I’m naïve, but I think we can find satisfactory answers from the powers that be without having to resort to such measures. The results garnered from an objective examination may well reveal “contract violations”…at least technically. Or, they might well have been mere deviations to address changing needs in our ever-changing health care environment.
What is disturbing is that it appears that the Hospital Board is unwilling (or unable) to provide answers to the basic questions posed here…coupled with the lack of access to the Board itself: Clamming up is not the way for them to proceed.
Thank you again for your valuable efforts
Dickford